What is Type 1 Diabetes?
Type 1 diabetes is a chronic autoimmune condition in which the body's immune system mistakenly attacks and destroys insulin-producing beta cells in the pancreas. Unlike Type 2 diabetes, Type 1 is not caused by lifestyle or diet and typically develops in childhood or adolescence, though it can occur at any age. Without insulin, the body cannot properly regulate blood glucose levels, leading to dangerously high sugar levels if untreated. People with Type 1 diabetes require lifelong insulin therapy to survive and manage their blood sugar. It is also referred to as insulin-dependent diabetes or juvenile diabetes. Early diagnosis and proper management are essential to prevent complications and support a healthy life.
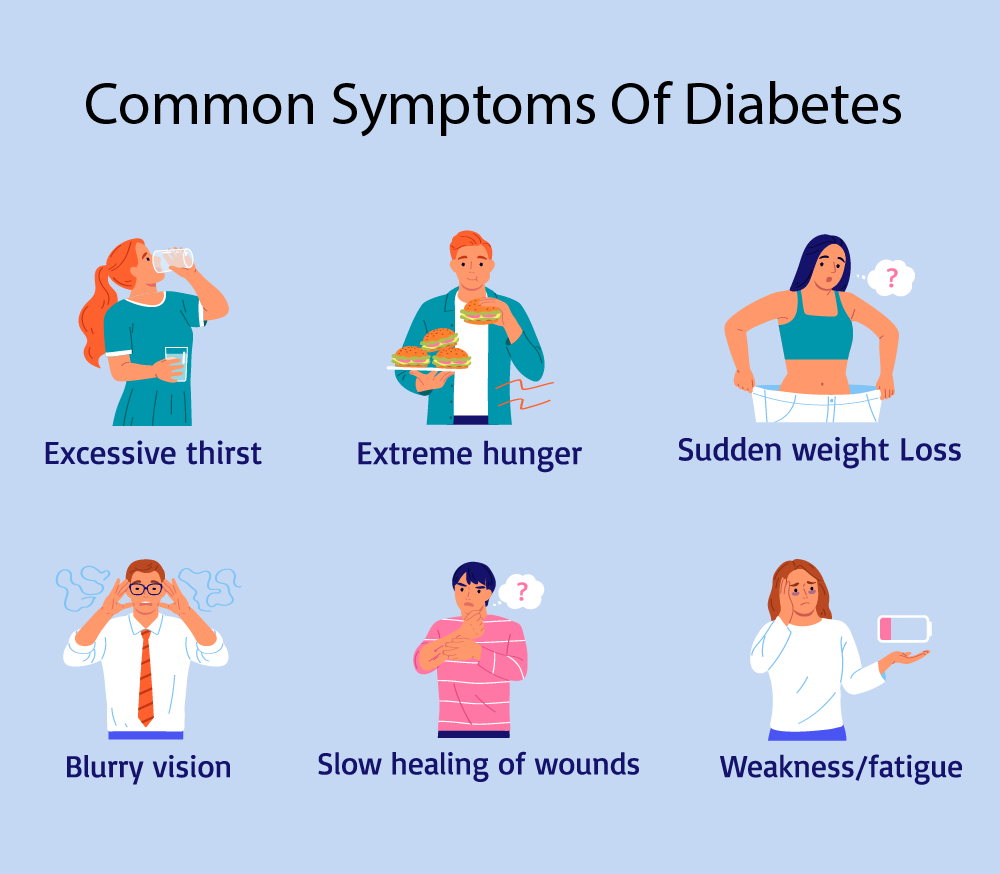
Symptoms and Causes
Common Symptoms:
- Increased thirst and frequent urination
- Extreme hunger
- Sudden weight loss
- Fatigue and weakness
- Blurred vision
- Mood changes or irritability
Causes:
The exact cause is unknown, but Type 1 diabetes is believed to be triggered by genetic factors combined with environmental triggers like viruses. The immune system's abnormal response leads to the destruction of insulin-producing cells.