What is a Convulsion?
Convulsions are sudden, involuntary muscle contractions and movements that occur during a seizure. They are usually a sign of abnormal electrical activity in the brain and may affect part of the body (focal seizure) or the entire body (generalized seizure). Convulsions may last from a few seconds to several minutes and are commonly associated with conditions like epilepsy, high fever in children (febrile seizures), head injuries, or neurological disorders. Some seizures are dramatic and obvious, while others may involve subtle symptoms like confusion or muscle twitching. Immediate medical attention is important, especially for first-time or prolonged episodes. Early diagnosis and consistent treatment can help manage symptoms and reduce recurrence. Understanding triggers and maintaining a seizure-safe environment is key to long-term care.
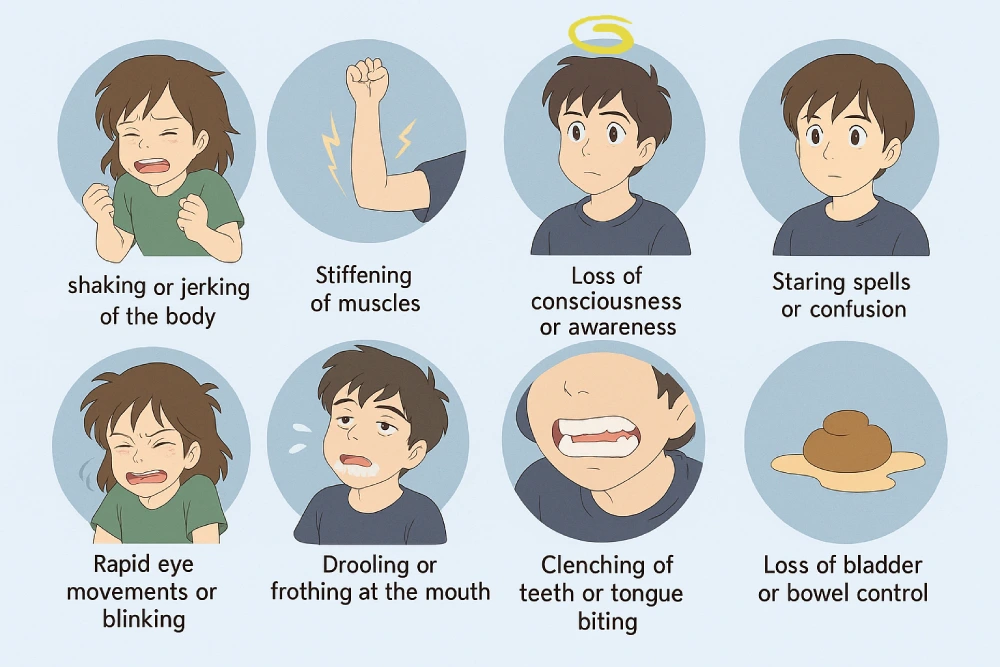
Common Symptoms and Signs
Symptoms of convulsions can vary depending on the type of seizure but may include:
- Sudden and uncontrollable shaking or jerking of the body
- Stiffening of muscles
- Loss of consciousness or awareness
- Staring spells or confusion
- Rapid eye movements or blinking
- Drooling or frothing at the mouth
- Clenching of teeth or tongue biting
- Loss of bladder or bowel control
After the seizure, the person may feel sleepy, confused, or have memory gaps.