What is Jaundice?
Jaundice is a medical condition characterized by a yellowish discoloration of the skin, eyes (sclera), and mucous membranes. It occurs due to elevated levels of bilirubin in the blood—a yellow pigment formed from the breakdown of red blood cells. Jaundice itself is not a disease but a sign of an underlying condition, usually involving the liver, gallbladder, or pancreas. It can affect people of all ages, from newborns to the elderly, and may indicate anything from mild liver stress to serious conditions like hepatitis, bile duct obstruction, or liver failure. Early diagnosis and treatment are crucial to manage the root cause and prevent complications. Additional symptoms may include dark urine, pale stools, and fatigue. Prompt medical attention is essential if jaundice appears suddenly or is accompanied by other warning signs.
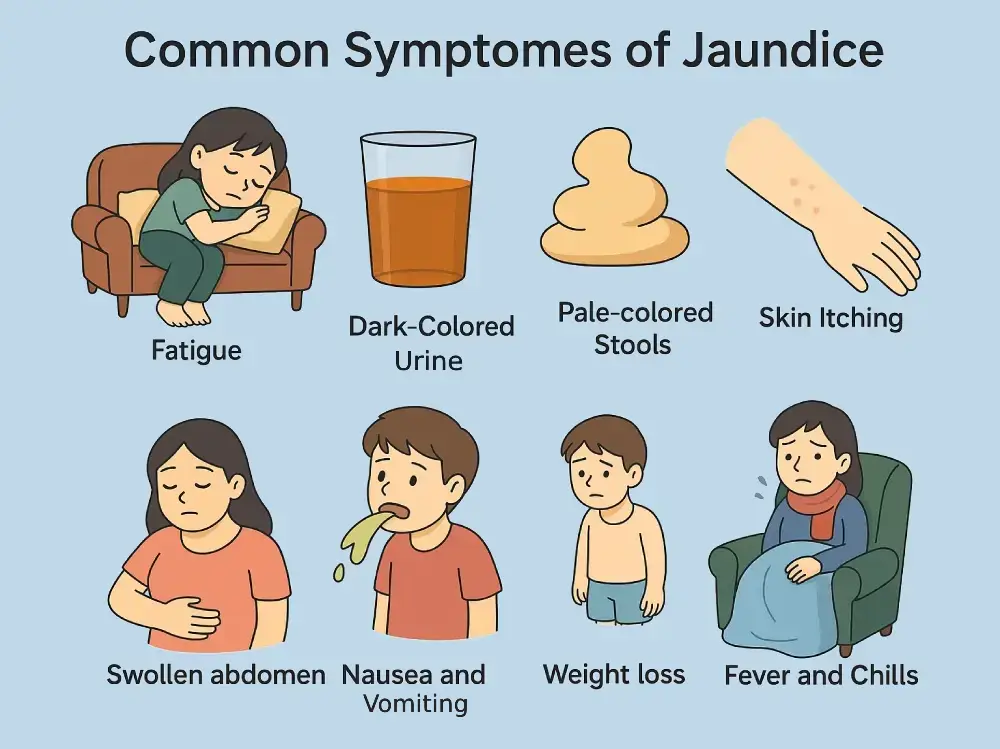
Common Symptoms and Signs
The most recognizable symptom is yellowing of the skin and eyes, but jaundice may also be accompanied by:
- Fatigue and weakness
- Dark-colored urine
- Pale or clay-colored stools
- Itchy skin (pruritus)
- Abdominal pain or swelling
- Nausea and vomiting
- Loss of appetite
- Weight loss
- Fever (in infections like hepatitis)
In infants, jaundice may appear within the first week of life and should be closely monitored.